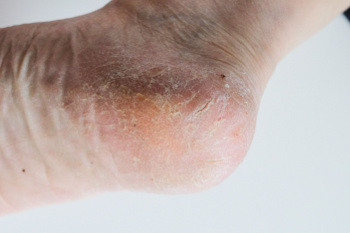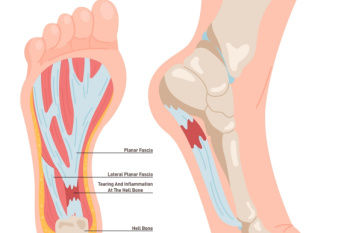
Plantar fasciitis is a common cause of heel pain, resulting from inflammation of the plantar fascia, which is the thick band of tissue that runs along the bottom of the foot and connects the heel bone to the toes. The condition typically causes a sharp, stabbing pain in the heel, particularly noticeable with the first steps in the morning or after periods of inactivity. Risk factors include prolonged standing, high-impact activities, obesity, and wearing unsupportive shoes. The pain usually lessens with movement but can return after long periods of standing or sitting. Treatment often involves stretching exercises, wearing proper footwear, and rest to reduce inflammation. In severe cases, orthotics or injections may be necessary. Plantar fasciitis can cause severe pain and can hinder completing daily activities. If you have heel pain, it is strongly suggested that you are under the care of a podiatrist who can accurately diagnose and treat plantar fasciitis.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Associates in Podiatry, PC. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in Pittsburgh-South Hills, and Pittsburgh-Bellevue, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
 Poor circulation
Poor circulation